Small step for Nature, giant leap across the gender gap: leading journal will make sex and gender reporting mandatory in research
Small step for Nature, giant leap across the gender gap: leading journal will make sex and gender reporting mandatory in research

Like in many aspects of life, there remains an undercurrent of sex bias against women in the STEM fields. And this bias has a negative impact on not only women, but men too – and those who don’t fit within a binary category.
Nature journals are now taking a leap for sex and gender equity with new reporting requirements, and it’s a welcome step in the right direction.
I work in the field of bioengineering, and researchers such as myself understand first hand the damage that can be done when sex and gender are not properly accounted for – and reported on – in research.
Nature journals a new policy
Come June, researchers who submit papers to a subset of the Nature Portfolio journals (see details here) will need to describe whether, and how, sex and gender are considered in study design.
If no sex and gender analyses were carried out, authors will need to clarify why. This will apply to work with human participants, as well as other vertebrate animals and cell experimental studies. So in the same way that ethics approval, clinical trials registration, or informed consent must be demonstrated where relevant, so too will consideration of sex and gender.
But what are sex and gender?
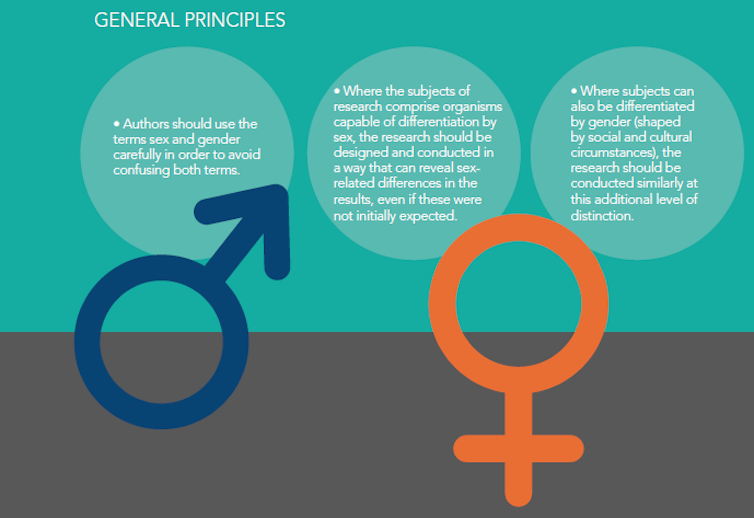
“Sex” and “gender” are terms that are often used interchangeably, but they are not the same thing. Sex refers to biological attributes, including genetics and reproductive organs. Gender is shaped by social and cultural influences, and may or may not align with an individual’s biological sex. Both sex and gender can influence our health.
Authors writing for Nature journals will also need to present “data disaggregated by sex and gender” where relevant. This means that rather than the (more often than not) approach of lumping male and female data together, it will need to be separated.
This is a necessary move towards unravelling differences between males and females. Researchers are encouraged to follow the Sex and Gender Equity in Research guidelines when designing research studies.
A lack of sex and gender considerations puts all at risk
Failure to conduct sex and gender-based analysis occurs across a range of disciplines. For example, in the field of engineering, car safety is designed for an average male body. This puts women at higher risk of injuries and death in the event of a crash.
Another example comes with facial recognition technologies, where studies have found error rates for “gender” classification are higher for females than for males (and also higher for darker-skinned people).
But medicine is one of the fields which is arguably most affected by a lack of sex and gender-based reporting.
Consequences can also be dire in medicine, where limited understanding of sex differences in biology and disease can directly impact on health. Our biological sex can make us more likely to suffer from certain diseases. It can make us respond differently to internal factors (such as the drugs we’re taking) or external factors (such as stress). It can even make us feel pain differently.
Our sex can influence the way we manifest symptoms for the same diseases, such as heart attack and stroke. For instance, symptoms of a women’s heart attack, such as fatigue, shortness of breath and nausea are labelled “atypical”, and lead to worse treatment and outcomes.
Large male biases have existed across all phases of medical research. There are many reasons for this. One is that female biology can often complicate things. A woman’s hormones fluctuate monthly and over her lifetime.
Another reason, historically, is protectionism. While it’s almost unbelievable (but true), women of “childbearing potential” were excluded from clinical trials from 1977 until 1993, to protect the “potential unborn” child.
On top of this is simply a lack of awareness, and a historical assumption (although this is finally changing) that what applies to men also applies to women.
Men can be harmed too
Sex-bias in medicine isn’t just putting women’s health at risk; it can also endanger men. For example, osteoporosis is up to four times more common in women. As a result, men are under-screened and under-diagnosed in this area – yet they have a higher chance of complication or death after breaking a bone.
The COVID-19 virus has also been shown to differ between sexes, with males being more likely to require intensive care treatment and having a higher risk of dying. These differences lead to questions around the reason(s) behind this.
What are the underlying sex differences causing this? Is it the immune system? Is it differences in hormones? Much is still unknown.
We must acknowledge the sex and gender gap
A big hurdle in narrowing the gender gap in healthcare is a lack of awareness that such a gap still exists. Sex and gender perspectives in health and biology need to be integrated into all aspects of medicine – from health research to medical education, through to clinical practise. This requires a concerted effort from governments, education systems and industry.
Many initiatives and institutes have been formed around the world to address issues around sex, gender and health, such as Canada’s Institute of Gender and Health. Australia and New Zealand need to align with other countries and implement sex and gender analysis in health and medical research.
And I, for one, echo Nature’s wise words: “Accounting for sex and gender makes for better science.”![]()
Kelly Burrowes, Senior Researcher, University of Auckland
This article is republished from The Conversation under a Creative Commons license. Read the original article.